Authors
The Challenge: Streamlining discharge and building collaboration
Many healthcare organisations are constantly striving to improve patient flow and optimise resource utilisation. There are challenges with discharge processes, leading to longer lengths of stay and a high number of care home discharge cases that could potentially be managed at a lower level in the community.
The root cause in the work we supported appeared to be a disconnect between acute care teams and the borough ToCH teams. Traditional workflows limited collaboration and often overlooked opportunities for a more efficient, patient-centred approach. Under pressure, staff felt restricted in their ability to explore new ways of working across organisational boundaries.
Recognising these challenges, we embarked on the ‘Shift Left’ project, a collaboration between hospital and community teams.
The Solution: ‘Shift Left’ Approach
PPL used the Model for Improvement and PDSA cycles to help the North Central London Integrated Care System improve patient and discharge outcomes. The ‘Shift Left’ project focused on reducing the need for high levels of care by improving discharge processes.
However, we understood that successful implementation hinged on more than just methodologies. We focused on ensuring strong staff engagement; empowering frontline staff from both acute and community settings to actively participate in the project. Leadership played a crucial role in providing the space and permission for cross-organisational collaboration. They championed the project’s goals and advocated for its importance. By creating a culture of open communication and valuing frontline input, we aimed to create lasting positive change that transcended traditional ways of working.
A local Change Team of senior MDT (multi-disciplinary team) members led the project, leading across the discharge process.
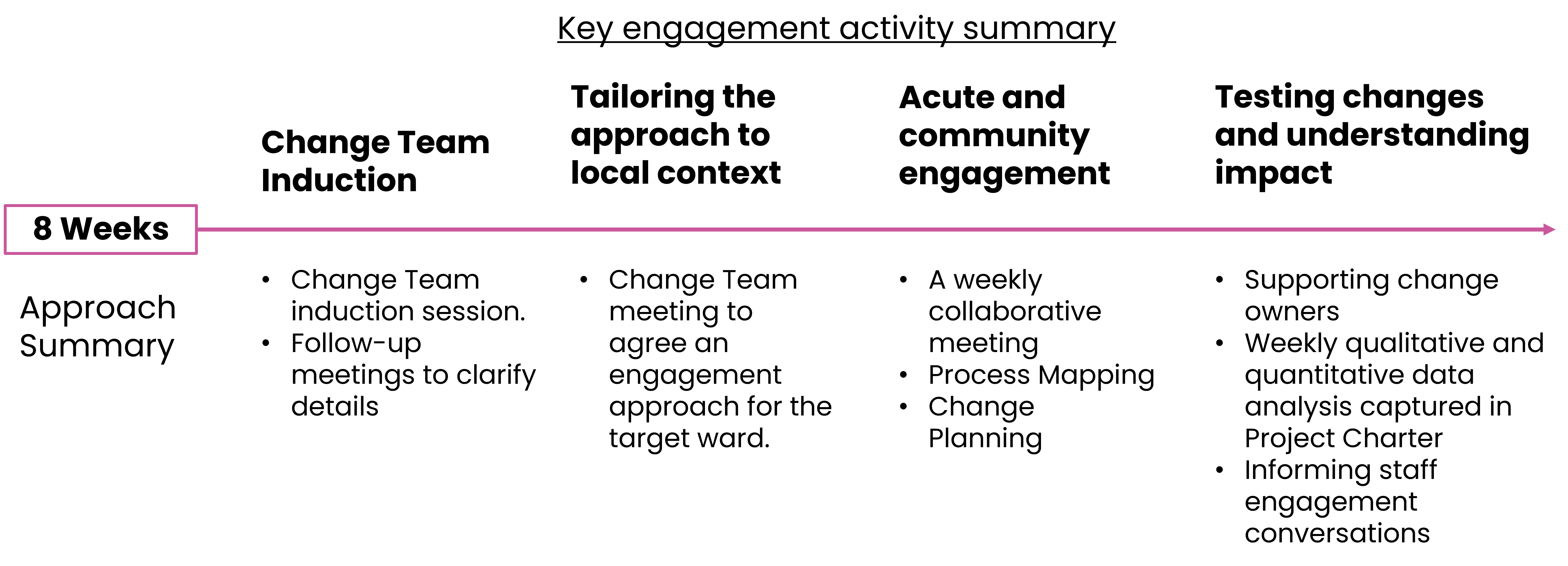
The project took place over eight weeks beginning with the Change Team’s induction, adapting strategies to local needs, involving both hospital and community settings, and concluding with testing and evaluating the changes. This structured approach ensured effective planning and continuous staff involvement, fostering ownership and engagement with the project outcomes.
The Change Team
To support the Change Team in their role, we provided thorough training in QI (quality improvement) methods and coaching, along with workshops to enhance their confidence in applying these principles and leading effective staff engagement meetings. Regular meetings offered the team opportunities to reflect, learn, and adjust the project’s direction based on staff feedback.
Boosting staff engagement
The ‘Shift Left’ project adopted a person-centred approach, supported by dedicated leadership. Senior Responsible Officers (SROs) from the local health and care system used their roles to inspire management, support the Change Team, and acknowledge staff contributions. Flexible scheduling of meetings during peak periods helped build trust and enhance engagement.
“Shift left is about helping people to return to the life they want to live.”
– Liam Furlong Barnet System Hospital Discharge Lead
Building connections
The ‘Shift Left’ project succeeded by focusing on teamwork, communication and transparency. The multi-disciplinary team (MDT), guided by PPL, ensured shared ownership of decision-making and the inclusion of diverse perspectives. The embedded MDT Change Team acted as a crucial link between leadership and frontline staff, facilitating open channels for real-time feedback and ensuring decisions reflected daily operational realities. A jointly developed driver diagram provided a visual and common roadmap, illustrating project goals, influential factors, and planned interventions. This collaborative approach reduced potential conflicts and aligned all participants towards unified objectives.
Outcomes: A paradigm shift in patient care
The ‘Shift Left’ project, guided by QI principles, achieved impressive results. The project promoted a culture of continuous improvement, empowering wards to independently drive and scale up successful activities beyond the initial project’s scope. This momentum signifies a broader shift in how patient discharge planning is approached.
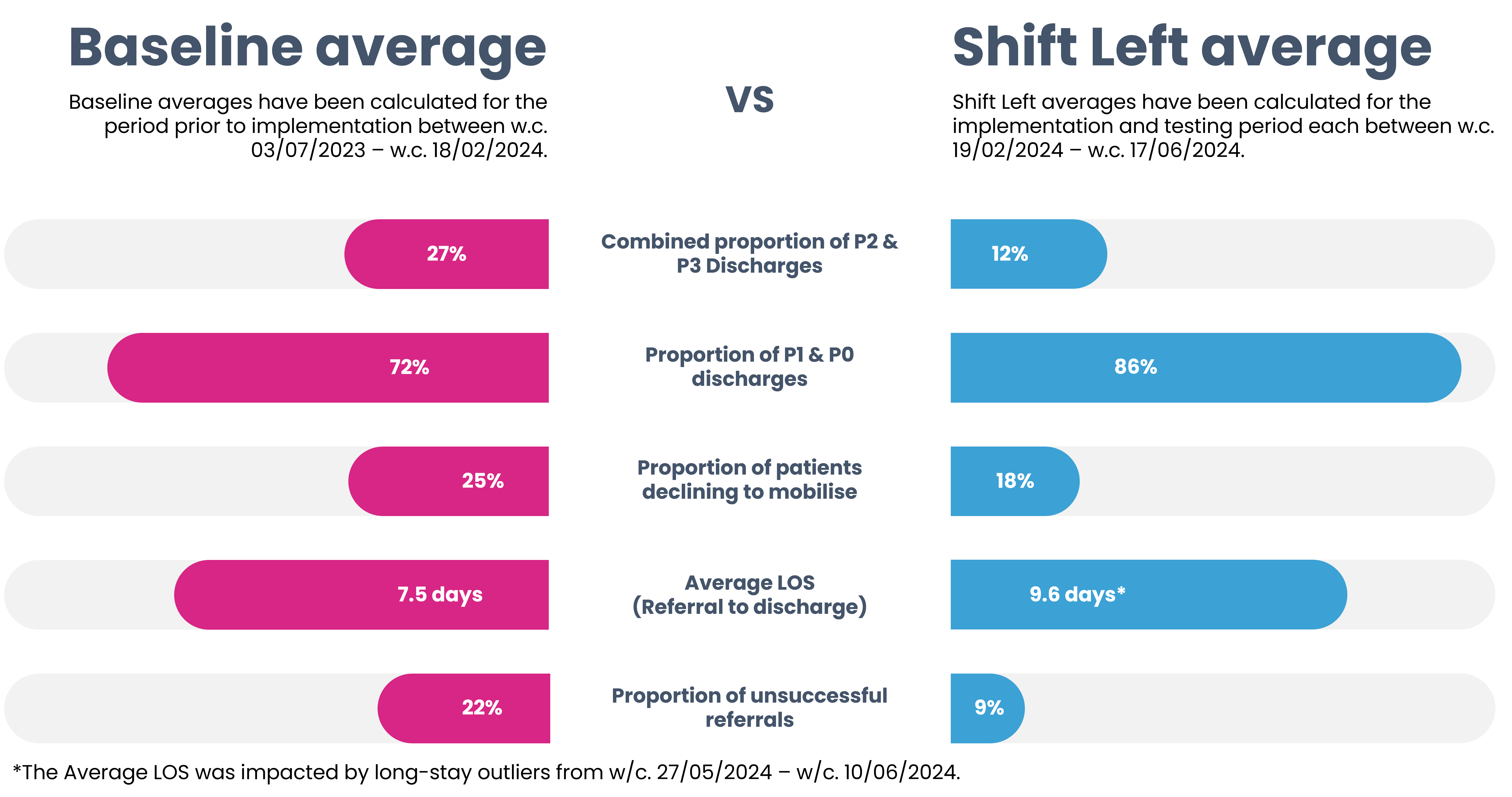
Data-driven decision-making, facilitated by QI methods, played a critical role in achieving these outcomes. The project’s success is reflected in the measured improvements:
- Reduced need for intermediate care: Fewer patients required post-discharge support from intermediate care services.
- Lower placement rates in nursing homes: More patients were able to return home safely and maximise their independence.
The ‘Shift Left’ project not only improved discharge processes but also served as a catalyst for broader system-wide change. Inspired by the project’s success, leadership discussions are underway to replicate these QI-driven approaches across the entire hospital system, bridging the gap between acute services and local community partners.
If you are interested in learning more about the Shift Left work outlined here or how it might apply to your area in healthcare, please contact:
Iyoni Ranasinghe Iyoni.Ranasinge@ppl.org.uk
Josh Lowe (Josh.Lowe@ppl.org.uk).






